Alzheimer’s doesn’t have to be your brain’s destiny, says neuroscientist and author of “Still Alice,” Lisa Genova. She shares the latest science investigating the disease — and some promising research on what each of us can do to build an Alzheimer’s-resistant brain.
Alzheimer’s is a type of dementia that causes problems with memory, thinking and behavior. Symptoms usually develop slowly and get worse over time, becoming severe enough to interfere with daily tasks.
Alzheimer’s is the most common form of dementia, a general term for memory loss and other cognitive abilities serious enough to interfere with daily life. Alzheimer’s disease accounts for 60 to 80 percent of dementia cases.
Alzheimer’s is not a normal part of aging. The greatest known risk factor is increasing age, and the majority of people with Alzheimer’s are 65 and older. But Alzheimer’s is not just a disease of old age. Approximately 200,000 Americans under the age of 65 have younger-onset Alzheimer’s disease.
Alzheimer’s worsens over time. Alzheimer’s is a progressive disease, where dementia symptoms gradually worsen over a number of years. In its early stages, memory loss is mild, but with late-stage Alzheimer’s, individuals lose the ability to carry on a conversation and respond to their environment. Alzheimer’s is the sixth-leading cause of death in the United States. Those with Alzheimer’s live an average of eight years after their symptoms become noticeable to others, but survival can range from four to 20 years, depending on age and other health conditions.
Alzheimer’s has no current cure, but treatments for symptoms are available and research continues. Although current Alzheimer’s treatments cannot stop Alzheimer’s from progressing, they can temporarily slow the worsening of dementia symptoms and improve quality of life for those with Alzheimer’s and their caregivers. Today, there is a worldwide effort underway to find better ways to treat the disease, delay its onset, and prevent it from developing. (http://www.alz.org/)

Transcript
“How many people here would like to live to be at least 80 years old? Yeah. I think we all have this hopeful expectation of living into old age. Let’s project out into the future, to your future “you’s,” and let’s imagine that we’re all 85. Now, everyone looks at two people. One of you probably has Alzheimer’s disease.
Alright, alright. And maybe you’re thinking, “Well, it won’t be me.” Then, OK. You are a caregiver. So — in some way, this terrifying disease is likely to affect us all.
Part of the fear around Alzheimer’s stems from the sense that there’s nothing we can do about it. Despite decades of research, we still have no disease-modifying treatment and no cure. So if we’re lucky enough to live long enough, Alzheimer’s appears to be our brain’s destiny.
But maybe it doesn’t have to be. What if I told you we could change these statistics, literally change our brain’s destiny, without relying on a cure or advancements in medicine?
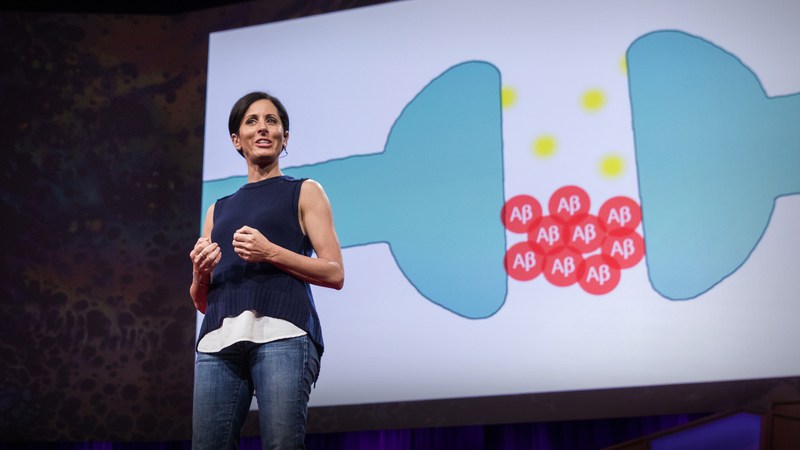
Let’s begin by looking at what we currently understand about the neuroscience of Alzheimer’s. Here’s a picture of two neurons connecting.

The point of connection, this space circled in red, is called the synapse. The synapse is where neurotransmitters are released. This is where signals are transmitted, where communication happens. This is where we think, feel, see, hear, desire … and remember. And the synapse is where Alzheimer’s happens. Let’s zoom in on the synapse and look at a cartoon representation of what’s going on.

During the business of communicating information, in addition to releasing neurotransmitters like glutamate into the synapse, neurons also release a small peptide called amyloid-beta. Normally, amyloid-beta is cleared away metabolized by microglia, the janitor cells of our brains. While the molecular causes of Alzheimer’s are still debated, most neuroscientists believe that the disease begins when the amyloid-beta begins to accumulate. Too much is released, or not enough is cleared away, and the synapse begins to pile up with amyloid-beta. And when this happens, it binds to itself, forming sticky aggregates called amyloid plaques.
How many people here are 40 years old or older? You’re afraid to admit it now. This initial step into the disease, this presence of amyloid plaques accumulating, can already be found in your brains. The only way we could be sure of this would be through a PET scan because at this point, you are blissfully unaware. You’re not showing any impairments in memory, language, or cognition … yet. We think it takes at least 15 to 20 years of amyloid plaque accumulation before it reaches a tipping point, then triggering a molecular cascade that causes the clinical symptoms of the disease. Prior to the tipping point, your lapses in memory might include things like, “Why did I come in this room?” or “Oh … what’s his name?” or “Where did I put my keys?”

Now, before you all start freaking out again because I know half of you did at least one of those in the last 24 hours — these are all normal kinds of forgetting. In fact, I would argue that these examples might not even involve your memory, because you didn’t pay attention to where you put your keys in the first place. After the tipping point, the glitches in memory, language and cognition are different. Instead of eventually finding your keys in your coat pocket or on the table by the door, you find them in the refrigerator, or you find them and you think, “What are these for?”
So what happens when amyloid plaques accumulate to this tipping point? Our microglia janitor cells become hyper-activated, releasing chemicals that cause inflammation and cellular damage. We think they might actually start clearing away the synapses themselves. A crucial neural transport protein called “tau” becomes hyperphosphorylated and twists itself into something called “tangles,” which choke off the neurons from the inside. By mid-stage Alzheimer’s, we have massive inflammation and tangles and all-out war at the synapse and cell death.
So if you were a scientist trying to cure this disease, at what point would you ideally want to intervene? Many scientists are betting big on the simplest solution: keep amyloid plaques from reaching that tipping point, which means that drug discovery is largely focused on developing a compound that will prevent, eliminate, or reduce amyloid plaque accumulation. So the cure for Alzheimer’s will likely be preventative medicine. We’re going to have to take this pill before we reach that tipping point before the cascade is triggered before we start leaving our keys in the refrigerator. We think this is why, to date, these kinds of drugs have failed in clinical trials — not because the science wasn’t sound, but because the people in these trials were already symptomatic. It was too late. Think of amyloid plaques as a lit match. At the tipping point, the match sets fire to the forest. Once the forest is ablaze, it doesn’t do any good to blow out the match. You have to blow out the match before the forest catches fire.
Even before scientists sort this out, this information is actually really good news for us, because it turns out that the way we live can influence the accumulation of amyloid plaques. And so there are things we can do to keep us from reaching that tipping point.

Let’s picture your risk of Alzheimer’s as a see-saw scale. We’re going to pile risk factors on one arm, and when that arm hits the floor, you are symptomatic and diagnosed with Alzheimer’s. Let’s imagine you’re 50 years old. You’re not a spring chicken anymore, so you’ve accumulated some amyloid plaques with age. Your scale is tipped a little bit.
Now let’s look at your DNA. We’ve all inherited our genes from our moms and our dads. Some of these genes will increase our risk and some will decrease it. If you’re like Alice in “Still Alice,” you’ve inherited a rare genetic mutation that cranks out amyloid-beta, and this alone will tip your scale arm to the ground. But for most of us, the genes we inherit will only tip the arm a bit. For example, APOE4 is a gene variant that increases amyloid, but you can inherit a copy of APOE4 from mom and dad and still never get Alzheimer’s, which means that for most of us, our DNA alone does not determine whether we get Alzheimer’s. So what does? We can’t do anything about getting older or the genes we’ve inherited. So far, we haven’t changed our brain’s destiny.
What about sleep? In slow-wave deep sleep, our glial cells rinse cerebral spinal fluid throughout our brains, clearing away metabolic waste that accumulated in our synapses while we were awake. Deep sleep is like a power cleanse for the brain. But what happens if you shortchange yourself on sleep? Many scientists believe that poor sleep hygiene might actually be a predictor of Alzheimer’s. A single night of sleep deprivation leads to an increase in amyloid-beta. And amyloid accumulation has been shown to disrupt sleep, which in turn causes more amyloid to accumulate. And so now we have this positive feedback loop that’s going to accelerate the tipping of that scale.

What else? Cardiovascular health. High blood pressure, diabetes, obesity, smoking, high cholesterol, have all been shown to increase our risk of developing Alzheimer’s. Some autopsy studies have shown that as many as 80 percents of people with Alzheimer’s also had cardiovascular disease. Aerobic exercise has been shown in many studies to decrease amyloid-beta in animal models of the disease. So a heart-healthy Mediterranean lifestyle and diet can help to counter the tipping of this scale.
So there are many things we can do to prevent or delay the onset of Alzheimer’s. But let’s say you haven’t done any of them. Let’s say you’re 65; there’s Alzheimer’s in your family, so you’ve likely inherited a gene or two that tips your scale arm a bit; you’ve been burning the candle at both ends for years; you love bacon, and you don’t run unless someone’s chasing you.
Let’s imagine that your amyloid plaques have reached that tipping point. Your scale arm has crashed to the floor. You’ve tripped the cascade, setting fire to the forest, causing inflammation, tangles, and cell death. You should be symptomatic of Alzheimer’s. You should be having trouble finding words and keys and remembering what I said at the beginning of this talk. But you might not be.
There’s one more thing you can do to protect yourself from experiencing the symptoms of Alzheimer’s, even if you have the full-blown disease pathology ablaze in your brain. It has to do with neural plasticity and cognitive reserve. Remember, the experience of having Alzheimer’s is ultimately a result of losing synapses. The average brain has over a hundred trillion synapses, which is fantastic; we’ve got a lot to work with. And this isn’t a static number. We gain and lose synapses all the time, through a process called neural plasticity. Every time we learn something new, we are creating and strengthening new neural connections, new synapses.
In the Nun Study, 678 nuns, all over the age of 75 when the study began, were followed for more than two decades. They were regularly given physical checkups and cognitive tests, and when they died, their brains were all donated for autopsy. In some of these brains, scientists discovered something surprising. Despite the presence of plaques and tangles and brain shrinkage — what appeared to be unquestionable Alzheimer’s — the nuns who had belonged to these brains showed no signs of having the disease while they were alive.
How can this be? We think it’s because these nuns had a high level of cognitive reserve, which is a way of saying that they had more functional synapses. People who have more years of formal education, who have a high degree of literacy, who engage regularly in mentally stimulating activities, all have a more cognitive reserve. They have an abundance and redundancy in neural connections. So even if they have a disease like Alzheimer’s compromising some of their synapses, they’ve got many extra backup connections, and this buffers them from noticing that anything is amiss.

Let’s imagine a simplified example. Let’s say you only know one thing about a subject. Let’s say it’s about me. You know that Lisa Genova wrote “Still Alice,” and that’s the only thing you know about me. You have that single neural connection, that one synapse. Now imagine you have Alzheimer’s. You have plaques and tangles and inflammation and microglia devouring that synapse. Now when someone asks you, “Hey, who wrote ‘Still Alice?'” you can’t remember, because that synapse is either failing or gone. You’ve forgotten me forever.
But what if you had learned more about me? Let’s say you learned four things about me. Now imagine you have Alzheimer’s, and three of those synapses are damaged or destroyed. You still have a way to detour the wreckage. You can still remember my name. So we can be resilient to the presence of Alzheimer’s pathology through the recruitment of yet-undamaged pathways. And we create these pathways, this cognitive reserve, by learning new things. Ideally, we want these new things to be as rich in meaning as possible, recruiting sight and sound and associations and emotion.
So this really doesn’t mean doing crossword puzzles. You don’t want to simply retrieve the information you’ve already learned, because this is like travelling down old, familiar streets, cruising neighborhoods you already know. You want to pave new neural roads. Building an Alzheimer’s-resistant brain means learning to speak Italian, meeting new friends, reading a book, or listening to a great TED Talk.
And if despite all of this, you are someday diagnosed with Alzheimer’s, there are three lessons I’ve learned from my grandmother and the dozens of people I’ve come to know living with this disease. Diagnosis doesn’t mean you’re dying tomorrow. Keep living. You won’t lose your emotional memory. You’ll still be able to understand love and joy. You might not remember what I said five minutes ago, but you’ll remember how I made you feel. And you are more than what you can remember.